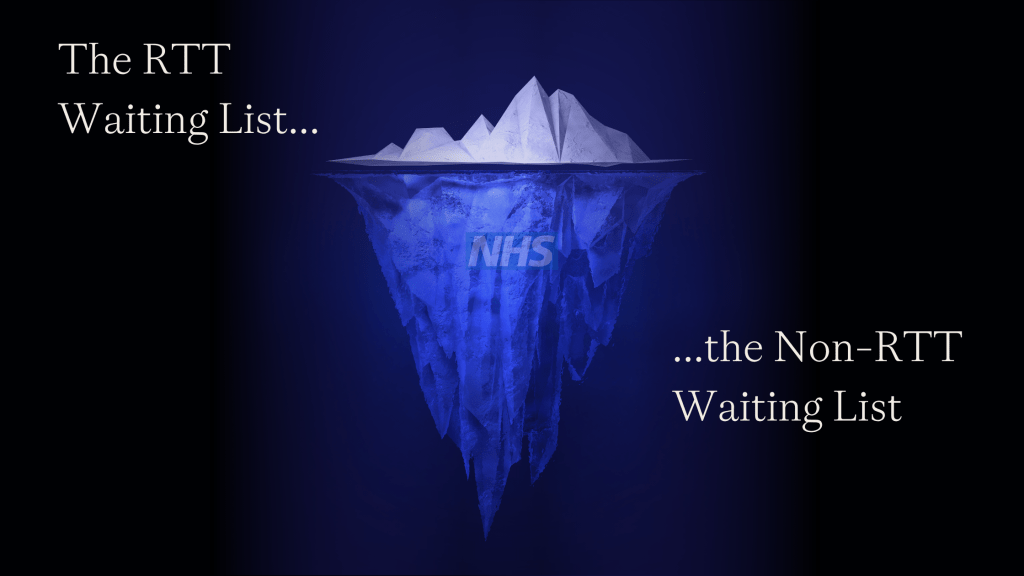
The NHS has never been under more pressure to recover elective care. Every Trust is measured on Referral to Treatment (RTT) waiting list performance, with targets to reduce NHS waiting lists, hit 18-week thresholds, and restore services to pre-pandemic levels.
These RTT figures are the numbers that NHS England monitors, that board meetings focus on, and that hospital leaders are held accountable for.
But while RTT performance is the headline story, it’s only the tip of the iceberg. Below the surface lies a larger, unreported backlog, one that carries greater clinical risk, higher patient safety concerns, and significant reputational exposure for Trusts.
That hidden backlog? Non-RTT Patient Tracking Lists (PTLs).
These are the patients who don’t count towards RTT but whose care is just as critical. And when things go wrong, it’s not RTT delays that make the headlines… it’s the patients lost in the Non-RTT system.
The Hidden Risk Below the Surface of NHS Waiting Lists
For every patient recorded on RTT NHS waiting lists, there are thousands more sitting on Non-RTT waiting lists, including:
✅ Surveillance Patients – Those awaiting routine follow-ups for cancer, ophthalmology, cardiology, and neurology. Missing these appointments can mean life-threatening disease progression going undetected.
✅ PIFU (Patient-Initiated Follow-Ups) – Patients who are expected to reach out when symptoms worsen. But what happens when they don’t? Who’s tracking those who should have called but never did?
✅ Ongoing Diagnostic Monitoring – Patients waiting for scans, biopsies, or other tests who are lost in scheduling systems, increasing the risk of missed or delayed diagnoses.
✅ Long-Term Condition Management – Patients with chronic conditions requiring scheduled check-ins that, when delayed, lead to deteriorating health and unplanned emergency admissions.
Unlike RTT, there’s no national target, no performance framework, and little governance oversight for these lists. They exist in Trust systems, but with no regulatory pressure to prioritise them, they are frequently neglected – until a serious incident forces them into the spotlight.
The PR Disaster Waiting to Happen
When things go wrong in elective care, it’s rarely RTT breaches that make the news.
Instead, it’s stories like:
⚠️ The patient who missed a routine cancer surveillance check and was diagnosed too late for treatment.
⚠️ The patient who was waiting for a follow-up cardiac scan that never got scheduled… until they arrived in A&E with a heart attack.
⚠️ The patient with a chronic neurological condition who was meant to be monitored every six months but got lost in the system for two years.
Unlike RTT breaches, which are seen as operational challenges, Non-RTT failures are seen as clinical failings, leading to real patient harm and institutional accountability.
If you’re a hospital leader, ask yourself:
-
Do we have a real-time view of our Non-RTT PTLs?
-
Are we proactively validating these waiting lists?
-
Do we have governance and oversight for Non-RTT pathways like we do for RTT?
If the answer to any of these is no, then it’s only a matter of time before a Non-RTT failure becomes your next crisis.
How NHS Trusts Can Get Ahead of the Problem
The solution isn’t to shift focus away from RTT, but to treat Non-RTT NHS waiting lists with the same level of urgency and scrutiny.
✅ Automate Validation & Risk Stratification – Use AI-driven tools to identify and flag high-risk patients before harm occurs.
✅ Ensure Full Data Assurance – Move beyond reactive reporting and make Non-RTT tracking an integral part of elective recovery strategies.
✅ Improve Governance & Oversight – Non-RTT PTLs need board-level attention, regular audits, and dedicated tracking systems.
✅ Break the Siloed Approach – Waiting list data, patient tracking, and clinical risk management need to be joined up, not treated as separate workstreams.
RTT may be the performance metric hospitals are judged on, but Non-RTT PTLs are where the real patient safety risks and reputational threats lie.
The Time to Act Is Now
The hospitals that proactively manage Non-RTT PTL will be the ones that:
🔹 Avoid serious incidents before they happen.
🔹 Prevent patient harm by ensuring timely follow-ups.
🔹 Build public trust by showing accountability for all waiting lists, not just RTT.
The iceberg is there. Will you take action before it hits?