Labour’s Health Secretary Wes Streeting has signalled patients will have increased access to choose where they are treated in future and defended the use of the private sector in helping bring down waiting lists.
This has always been a controversial notion but today we would like to highlight another reason that is not mentioned at all in the debate – data quality.
NHS organisations are managed robustly on the quality of data they provide about what is happening to their patients. Evidence shows private providers simply aren’t managed in the same way or to the same standard as NHS providers.
Let’s start by looking at the standard arguments against using private providers:
- Cost and Value for Money
- Higher Costs: Critics argue that private sector treatments often come at a higher cost than NHS-provided services. While private hospitals might be able to handle procedures quickly, the per-patient expense can be higher, especially when contracts aren’t tightly managed.
- Hidden Fees and Contracts: There can be issues with transparency around private hospital billing and additional costs. Critics point out that the final cost to the NHS might not always be clear at the start, leading to budget overshoots.
- Long-Term Investment: Some believe that outsourcing to the private sector is a short-term fix that prevents long-term investment in NHS infrastructure. Instead of paying for external services, the argument is that funds could be used to expand capacity within the NHS itself.
- Quality of Care and Oversight
- Variable Quality: While some private hospitals have excellent standards, others might not match NHS levels for safety, especially when it comes to emergency response. There have been cases where private hospitals have not met the same stringent standards of oversight as NHS trusts, raising concerns about patient safety.
- Fragmentation of Care: Treating NHS patients in private hospitals can sometimes lead to a lack of continuity in care. For instance, patients might be treated in a private hospital but have follow-up care or complications managed by the NHS, which can create communication gaps and fragmented care pathways.
- Limited Specialisation: Private hospitals often focus on routine, elective procedures and may not have the same level of specialised care that NHS hospitals offer. If something goes wrong or complications arise, patients might need to be transferred back to NHS facilities, which can disrupt care.
- Equity and Access Issues
- Two-Tiered System: Critics worry that using private hospitals can exacerbate inequalities, creating a two-tiered system where those who can afford to pay can access faster treatment while others wait. The concern is that this undermines the core NHS principle of equitable care for all, based on need rather than ability to pay.
- Queue-Jumping: Even when treatments are funded by the NHS, critics argue that using private hospitals to ease waiting lists can be seen as a form of queue-jumping. There’s a concern that this might not address the underlying issues causing delays in the NHS and could incentivise patients to seek private care for quicker access.
- Capacity and Workforce Impact
- Impact on NHS Staff: By diverting patients to private hospitals, critics argue that it can take away cases from NHS staff, potentially affecting their training and skill development. Surgeons and other clinicians need a steady flow of cases to maintain their skills, and too much reliance on private providers could weaken this.
- Staffing Shortages: The NHS already faces significant staffing shortages, and some argue that relying on private providers may exacerbate this. NHS-trained staff are often recruited by private hospitals, which can drain resources from the NHS and create a loop of dependence on the private sector.
- Short-Term Fix: Using private hospitals can sometimes be seen to quickly bring down waiting lists without addressing the core issues of NHS capacity and workforce shortages. Critics argue that this can be a temporary solution that doesn’t lead to sustainable improvements.
All these factors contribute to a reluctance to use private capacity for NHS patients. However, we believe there is a fifth issue which is rarely debated: DATA QUALITY.
Data Quality in the Private Sector
We’ve looked at how the private sector compares to the NHS on data quality and the results are not good.
For NHS Trusts who are managing over 7m patients there are 640k data quality errors – 8.5%.

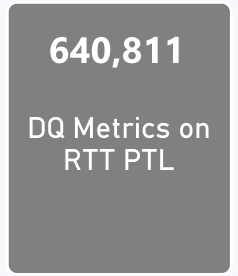

Figure 1: Data Quality issues on the RTT waiting list for NHS Trusts
When we look at the same measures for the private sector, they are significantly worse, Private Providers percentage of data quality issues are more than double that of NHS Trusts.

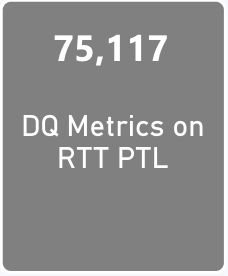

Figure 2: Data Quality issues on the RTT waiting list for private hospitals
What’s even more troublesome is the errors themselves. When comparing the specific errors NHS Trusts are experiencing, they are often less serious than the errors showing up in private providers. So not only is the problem more than double in private providers, but the errors themselves are more serious.
So what?
Data quality problems on waiting lists have been consistently proven to have negative impacts on patients. This could range from delays leading to worse outcomes, right through to incorrect information causing harm.
I read an article recently where the Association of Optometrists were arguing for more use of private sector capacity. To quote a famous line from the Profumo affair “well they would, wouldn’t they”. No consideration at all was given to how poor these provider’s data quality was.
Put simply, the levels of data quality issues in private providers are in my view, not acceptable. As a minimum I would expect them to be equivalent to NHS hospitals but in reality they should be much better than NHS hospitals given the extra resource the private sector can bring.
In short, if I was being transferred to a private provider that had a 17% error rate I wouldn’t choose to go there.
My two takeaways would be:
- If private providers want to take on more NHS patients, then they should ensure their data is of the highest quality.
- The NHS should refuse to allow patients to be sent to private providers with high data quality error rates.
If you would like to know more about our analysis or need help with data quality errors please GET IN TOUCH